Childhood Cancer Awareness Month: Early Signs, Treatments, and Hope — A Hyderabad Parent’s Guide (2025)

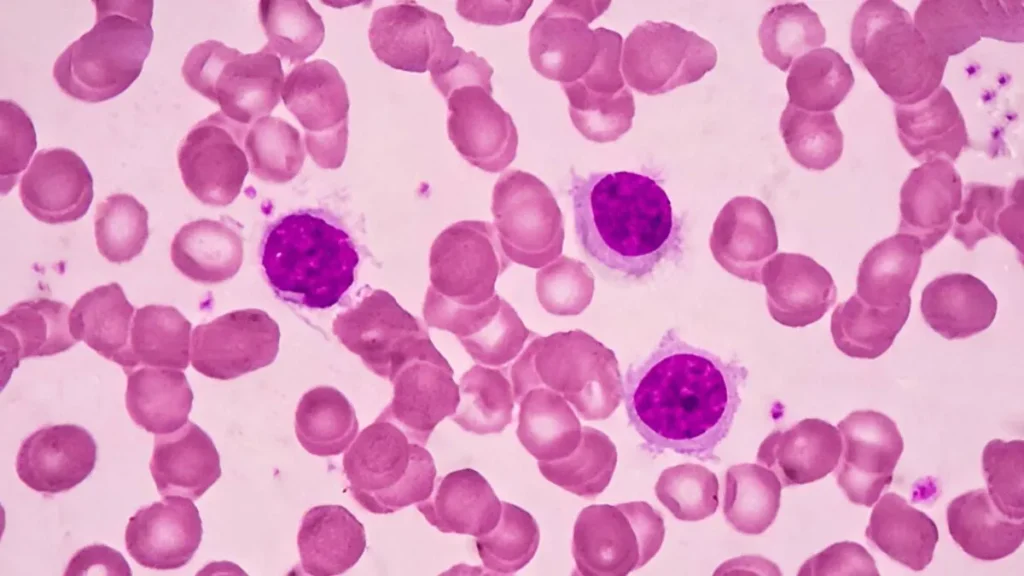
By Dr. Saadvik Raghuram, HOD Medical Oncology, Hyderabad Why Childhood Cancer Awareness Month Matters Childhood cancers are not rare for the families they affect—and timely referral to a specialist team changes outcomes. Globally, the WHO Global Initiative for Childhood Cancer aims to raise survival to at least 60% by 2030, potentially saving 1 million children over a decade. In India, cancers in children (0–14 years) account for ~4% of all cancers, with lymphoid leukemia the most common childhood malignancy reported by national registries. The Most Common Childhood Cancers While cancer types in children differ from adults, three groups dominate the 0–14 age range: These patterns are consistent across global and Indian data. Early Warning Signs Parents Shouldn’t Ignore Children can’t always articulate symptoms, and early signs may mimic infections. Use the SILUAN checklist, developed to prompt early evaluation and referral: What to do: If these signs persist beyond 1–2 weeks, do not self-medicate. Request a prompt referral to our oncology team. How Childhood Cancers Are Diagnosed Modern Treatment: More Curative, More Precise Most children receive multimodality care: Treatment plans follow evidence-based pediatric pathways (PDQ) and are adapted to each child’s biology and risk. The Good News: Survival Is Rising—But Survivorship Needs Care Thanks to protocol-driven therapy and supportive care, ~85% of children in high-resource settings live ≥5 years after diagnosis. Yet many survivors face late effects—from cardiac or endocrine issues to fertility concerns and learning challenges—requiring long-term, structured follow-up. Survivorship best practice: Create a written care plan aligned to Children’s Oncology Group (COG) Survivorship Guidelines and update it through adolescence and adulthood. Practical FAQs for Families in Hyderabad 1) Can routine vaccines continue during chemotherapy? Some inactivated vaccines may be given on schedule; live vaccines are typically postponed until immune recovery. Always individualize with your oncology team. (For general principles, oncologists follow national and CDC-aligned immunization precautions.) 2) Does diet “treat” cancer? No diet cures cancer. However, medically guided nutrition improves tolerance to therapy, growth, and immunity. Work with your oncology dietitian. 3) Are all fevers emergencies? For a child on chemotherapy, fever is an emergency. Seek care immediately—suspected febrile neutropenia needs urgent antibiotics. 4) When is a second opinion helpful? For rare tumors, relapsed disease, or when advanced radiation (e.g., proton therapy) might reduce long-term side-effects, a second opinion and multidisciplinary tumor board review are valuable. India & Global Context: Why Early Referral Saves Lives How We Care: Dr. Saadvik’s Oncology Philosophy If your child has persistent warning signs, book an urgent oncology assessment. Early action saves lives. A 10-Point Parent Checklist References If you’re in Hyderabad and worried about persistent symptoms in your child, contact Dr. Saadvik Raghuram for a same-week oncology review, evidence-based treatment planning, and a comprehensive survivorship roadmap. Disclaimer: This article is for education and should not replace medical advice. For emergencies (fever during chemotherapy, uncontrolled bleeding, breathing difficulty), seek immediate hospital care.
How Late Night Scrolling Can Increase Cancer Risk: Insights from Dr. Saadvik Raghuram, HOD Medical Oncology, Arête Hospital

In today’s digital age, staying up late with a phone in hand has almost become a nightly ritual. However, what may seem like harmless late-night scrolling could, in fact, be silently harming your health. As the Head of Medical Oncology at Arête Hospital, I, Dr. Saadvik Raghuram, frequently counsel patients on the profound impact of lifestyle habits on cancer risk. One of the most overlooked factors is disruption of circadian rhythm caused by poor sleep hygiene and excessive screen use at night. The Science of Melatonin and Circadian Rhythm The human body follows a natural circadian rhythm, an internal 24-hour clock that regulates essential biological processes including sleep, metabolism, and hormone secretion. Central to this rhythm is melatonin, a hormone secreted by the pineal gland during darkness, which signals the body that it is time to rest. When you scroll your phone late at night, the blue light emitted by screens suppresses melatonin secretion. A study published in the Journal of Clinical Endocrinology & Metabolism (2011) found that exposure to blue light as short as 2 hours at night significantly reduced melatonin production. This chronic suppression of melatonin does more than just cause poor sleep—it disrupts the circadian rhythm, which is increasingly being linked to cancer risk. Circadian Disruption and Cancer: What Research Shows Multiple studies over the last two decades have highlighted the association between circadian rhythm disruption and cancer development: Why Hyderabad Patients Should Be Concerned Hyderabad is a thriving IT hub, with thousands of professionals working irregular hours, late-night shifts, or spending excessive screen time even after work. As a practicing oncologist in Hyderabad, I see many young patients who are unaware that their lifestyle could be silently elevating their cancer risk. In a city where access to sunlight during workdays is limited and screen exposure is high, melatonin suppression is a growing concern. Pair this with sedentary lifestyles, stress, and irregular eating patterns, and the risk amplifies. Practical Steps to Protect Your Health While we cannot eliminate technology from our lives, we can adopt simple, evidence-based steps to safeguard circadian health: Conclusion Late-night scrolling may feel harmless, but over time it can disrupt melatonin levels, disturb circadian rhythm, and increase cancer risk. As the Best Oncologist in Hyderabad and Best Cancer Doctor in Hyderabad, my goal is to raise awareness about how everyday habits can influence long-term cancer outcomes. Your health is not only about advanced treatments—it is equally about prevention through mindful living. By protecting your body’s natural clock, you are also protecting yourself from potential cancer risks. About the Author Dr. Saadvik Raghuram is the Head of Medical Oncology at Arête Hospital, Hyderabad. Recognized as one of the Best Cancer Doctors in Hyderabad, he specializes in evidence-based cancer care with a focus on prevention, early detection, and advanced treatment options.
Low Vitamin D and Cancer: What Patients in Hyderabad Should Know !

(By Dr. Saadvik Raghuram, HOD – Medical Oncology, Arête Hospital | often consulted as the best oncologist in Hyderabad and a trusted best cancer doctor in Hyderabad) Quick Summary (for patients) What is Vitamin D and Why Does it Matter in Oncology? Vitamin D (D₂/D₃) is a hormone-like nutrient essential for bone health, immune modulation, and cellular growth control. Both D₂ and D₃ raise blood 25-hydroxyvitamin D [25(OH)D], with D₃ generally raising it more. From a cancer perspective, laboratory studies suggest vitamin D signaling can influence cell proliferation, differentiation, apoptosis, and immune responses—all relevant to tumor biology. However, real-world clinical outcomes must come from randomized trials, not only lab or observational data. Does Low Vitamin D Increase Cancer Risk? Observational Evidence Many observational studies link lower 25(OH)D levels with higher risks of certain cancers (e.g., colorectal). But such studies can be confounded by lifestyle, sun exposure, diet, and illness. That’s why oncologists rely on randomized trials to guide patient care. Randomized Clinical Trials & Meta-Analyses (What We Trust Most) Bottom line: Low vitamin D correlates with worse outcomes, but supplementing everyone to prevent cancer isn’t supported by strong trial evidence. How Common is Vitamin D Deficiency in India? Systematic reviews across South Asia (including India) show deficiency rates often exceed 50%, especially among women. Causes include indoor lifestyles, sun avoidance, skin pigmentation, air pollution, and diet. India’s 2024 Dietary Guidelines for Indians (ICMR-NIN) emphasize adequate sunlight exposure as part of national guidance. Should You Get Tested for Vitamin D? General Population The USPSTF finds insufficient evidence to recommend routine screening for asymptomatic adults. Who Should Consider Testing? What Levels Are “Low,” “Enough,” and “Too Much”? Tolerable upper intake level (UL): 4,000 IU/day for adults and children ≥9 years, without supervision. What Do the Latest Guidelines Say? The Endocrine Society’s 2024 guideline recommends: Practical Advice for Patients in Hyderabad For Patients Already Diagnosed with Cancer FAQs Is Vitamin D a “Cancer Shield”? No. RCTs show no reduction in overall cancer incidence with supplementation. What Dose Should I Take? Only as advised by your clinician. Do not exceed 4,000 IU/day unless supervised. Should Every Hyderabadi Test Vitamin D Levels? Not necessarily—only if you have risk factors or symptoms. Can I Rely on Sun Exposure Alone? Often not—urban lifestyles, air pollution, skin type, and clothing reduce UV-B absorption. Diet and supplements may be necessary. Professional Note from Dr. Saadvik Raghuram Y As a medical oncologist in Hyderabad, my approach is evidence-first: (If you’re searching for the best oncologist in Hyderabad or the best cancer doctor in Hyderabad, Dr. Saadvik Raghuram provides personalized, research-driven care.)
How Weight Gain Raises Uterine Cancer Risk – Early Signs You Shouldn’t Miss

Uterine cancer risk is rising with obesity, yet awareness remains low. Hormonal imbalance from excess weight can trigger cancer. Early detection, weight management, and regular check-ups are key to prevention Uterine cancer, among the most common cancers in women, often builds up with little warning. Behind many of these cases is a growing risk factor—literally and statistically: obesity. While this link is well understood in clinical settings, public awareness still lags far behind. With obesity rates increasing steadily—especially in women in their 30s and 40s—the danger is no longer abstract. It’s current. It’s widespread. And for many, it remains unspoken until a diagnosis arrives. How Weight Disrupts Hormonal Balance Carrying excess body fat affects more than joints or metabolism—it alters hormones. Fat tissue produces estrogen, and in women who aren’t ovulating regularly (a common occurrence in obesity), estrogen levels remain unchecked. Without enough progesterone to counterbalance it, the uterine lining thickens in an unhealthy way. Over time, this hormonal imbalance can lead to cellular changes that raise cancer risk. Among the clearest examples is endometrial cancer, which has shown strong associations with obesity. Research shows that women with obesity may face up to three times the risk compared to those with lower body weight. It Doesn’t Always Begin with Symptoms – (Weight Gain Raises Uterine Cancer Risk) Early signs aren’t always obvious. Irregular bleeding, spotting between cycles, or bleeding after menopause can be early warnings—but they’re easy to miss or dismiss. For younger women especially, these symptoms may not feel serious. Carrying excess weight can blur early warning signs and may also change how the body reacts when illness begins. Many women also miss regular check-ups, especially when they feel healthy. But gynaecological screenings are often the only way to catch early changes. These appointments matter—even when nothing seems wrong. Delayed detection often means more aggressive treatment is needed later on. Where Awareness Can Save Lives Weight management isn’t about appearance. It’s about reducing real, measurable risk. Staying alert to unusual changes in menstrual health, keeping regular check-ups, and being open with doctors about concerns all contribute to early diagnosis. Even small weight loss can have a protective effect—restoring hormonal balance and improving overall reproductive health. Lifestyle changes, made consistently, can make a difference in prevention. What Needs to Change Uterine cancer can be treated effectively when caught early. But the first step is knowing the risks—and not dismissing them. Understanding how weight affects hormone health isn’t about judgment. It’s about giving women the information they need to protect their bodies before symptoms ever appear. If you have any doubt contact us
Bone Cancer Awareness Month: The Latest Research, Early Detection & Expert Care in Hyderabad
Bone Cancer Awareness Month: The Latest Research, Early Detection & Expert Care in Hyderabad By Dr. Saadvik Raghuram | HOD Medical Oncology, Arête Hospitals | Hyderabad Every July, the global oncology community observes Bone Cancer Awareness Month, a time to focus on a group of rare but serious malignancies that often go undetected until advanced stages. As a practicing medical oncologist in Hyderabad, I believe it’s imperative to highlight the latest clinical insights, early detection strategies, and advancements in bone cancer treatment that can potentially save lives. What is Bone Cancer? Bone cancer refers to malignant tumors that originate in bone tissue, distinct from cancers that spread (metastasize) to the bone from elsewhere. While rare, primary bone cancers can be aggressive and require specialized, multidisciplinary care. Primary Bone Cancers Include:• Osteosarcoma – The most common type, particularly in adolescents and young adults.• Chondrosarcoma – Arises from cartilage-producing cells; more common in adults over 40.• Ewing Sarcoma – Affects children and young adults, often presenting in the pelvis, femur, or ribs. According to GLOBOCAN 2023, bone sarcomas account for less than 0.2% of all new cancer cases globally, yet their burden is disproportionately high in terms of morbidity due to late diagnosis and aggressive progression. Recent Research and Advances in Bone Cancer (2022–2024) A 2022 meta-analysis published in Cancer Discovery found that next-generation sequencing (NGS) in sarcomas revealed targetable mutations in 34% of cases. This opens the door to personalized therapy for bone tumors.• For instance, IDH1/2 mutations in chondrosarcoma are being explored as targets for investigational agents.• TP53 and RB1 mutations in osteosarcoma are being studied to predict prognosis and chemotherapy resistance. Source: Barretina et al., Cancer Discovery, 2022; “Genomic Landscape of Sarcomas” Though traditional sarcomas have been considered immunologically “cold”, research is evolving. A Phase II trial by MD Anderson (2023) demonstrated partial responses in patients with advanced bone sarcoma treated with nivolumab plus ipilimumab, showing a disease control rate of 28%. Reference: Tawbi et al., Lancet Oncology, 2023 A 2022 clinical review in The Lancet Oncology reported that proton therapy reduced radiation-induced toxicities by up to 60% compared to conventional photon therapy in pediatric Ewing sarcoma patients, without compromising tumor control. Reference: Merchant TE et al., Lancet Oncology, 2022 Early Detection: A Clinical Priority in India Early diagnosis remains the most critical factor in improving survival outcomes. However, in India, patients with primary bone tumors often present 6–8 months late, largely due to lack of awareness and misdiagnosis. A multicenter Indian study (AIIMS + TMH, 2023) showed that nearly 40% of primary bone sarcomas were initially misdiagnosed as infections or trauma-related injuries. Red Flag Symptoms to Watch:• Persistent bone pain, especially at night or during activity• Swelling or palpable mass near a joint or long bone• Spontaneous fractures• Unexplained fatigue, weight loss• Pain not relieved by rest or common analgesics Why Choose Dr. Saadvik Raghuram for Bone Cancer Care in Hyderabad? I specialize in solid tumor oncology, including sarcomas and rare cancers. My focus is on: Evidence-based protocolsTumor board-based collaborative decisionsPersonalized patient education and support Being recognized among the best oncologists in Hyderabad, I strive to bring cutting-edge oncology to every patient—whether it’s a 14-year-old with osteosarcoma or a senior adult battling chondrosarcoma. July: What You Can Do for Bone Cancer Awareness Month • Share this blog to spread awareness• Encourage friends and family to seek prompt evaluation for persistent bone pain• Follow @DrSaadvikRaghuram for the latest cancer education• Support sarcoma research initiatives Get Expert Help If you or your loved one is experiencing symptoms or has been recently diagnosed, schedule a consultation for treatment plan: Dr. Saadvik Raghuram | HOD Medical Oncology, Arête Hospitals | Hyderabad
What Are Rare Cancers and Why Do They Demand Urgent Attention
When people talk about cancer in India, the focus is mostly on the more common types: breast cancer, lung cancer, and cervical cancer. These are the ones that come up in awareness drives and are mentioned in public health discussions. But there’s another side to the picture. Rare cancers, such as sarcomas and certain blood-related malignancies; leukaemias, lymphomas, and multiple myelomas, often go undetected. And unfortunately, many of these are only picked up when the disease has already progressed. Read More
How Risk-Reducing Surgeries Help Young BRCA Carriers with Breast Cancer Live Longer by Dr. Saadvik Raghuram Y

Understanding the Risk If you’re a young woman diagnosed with breast cancer and carry a BRCA1 or BRCA2 mutation, you’re at a higher risk not just for a second breast cancer—but also ovarian cancer. But here’s the good news: science now confirms that certain preventive surgeries can significantly improve survival. A large international study (published in The Lancet Oncology, 2025) tracked over 5,000 women under age 40 with BRCA mutations and breast cancer—and the results were clear. What Are Risk-Reducing Surgeries? 1. Risk-Reducing Mastectomy (RRM):Removal of the healthy breast to prevent second breast cancers.2. Risk-Reducing Salpingo-Oophorectomy (RRSO):Removal of the ovaries and fallopian tubes to prevent ovarian cancer. What This Means for You If you’re a BRCA1/2 mutation carrier and have been diagnosed with breast cancer at a young age:• Risk-reducing mastectomy helps prevent new breast cancers and extends survival.• Ovarian removal (RRSO) significantly improves overall survival—especially for BRCA1 carriers and those with HER2-positive breast cancer. Final Thoughts This study reinforces the power of preventive surgery when tailored to your unique risk profile. These aren’t just life-saving—they’re life-extending. Consult Dr. Saadvik Raghuram to understand your BRCA risk and treatment options
Weight Gain and Late Pregnancy: Hidden Breast Cancer Risk Factors Every Woman Should KnowInsights from Dr. Saadvik Raghuram – Leading Medical Oncologist in Hyderabad

In today’s fast-paced world, many women delay pregnancy or experience weight gain in adulthood due to lifestyle demands. While these decisions may be common, they can have long-term health implications—particularly concerning breast cancer risk. As the best oncologist in Hyderabad with extensive experience in treating breast cancer, I believe it’s crucial to raise awareness about how these two factors—adult weight gain and late age at first pregnancy—can significantly elevate breast cancer risk. Understanding the Link Between Weight Gain and Breast Cancer Excess body weight is more than just a number on a scale. Fat tissue acts as a hormone-producing organ, increasing estrogen levels in the body. Prolonged estrogen exposure is a well-known contributor to hormone-positive breast cancer, the most common form of the disease. As a breast cancer specialist in Hyderabad, I regularly see how lifestyle-driven weight gain—especially after the age of 20—can contribute to a metabolic and hormonal environment that supports cancer development. This includes chronic inflammation, insulin resistance, and elevated growth factors, all of which can stimulate tumor growth. Why Timing of Pregnancy Matters Early pregnancy—especially before age 30—triggers cellular changes in breast tissue that lower lifetime breast cancer risk. When pregnancy is delayed, these protective changes occur later or not at all in women who remain child-free. Many women in Hyderabad and around the world are choosing to start families later due to personal and professional goals. While entirely valid, it’s important to understand that delayed pregnancy, when combined with significant adult weight gain, can compound the risk of developing breast cancer. The Combined Risk In my clinical experience as a top cancer doctor in Hyderabad, I’ve observed that women with both risk factors—substantial weight gain and delayed motherhood—often face a higher chance of being diagnosed with breast cancer in their 40s or 50s. These women may also experience more complex treatment journeys, particularly when cancers are diagnosed at a more advanced stage. How to Reduce Your Breast Cancer Risk and Know Breast Cancer Risk Factors Breast cancer prevention is not just possible—it’s actionable. Here are my evidence-based recommendations: Regular exercise, strength training, and a balanced diet can significantly reduce cancer risk. Even a 5-10% weight loss in overweight women can lower the likelihood of breast cancer. If you plan to delay pregnancy, discuss your breast health with your gynecologist or oncologist. Personalized screenings and lifestyle planning can be valuable tools for prevention. Both alcohol and tobacco are established cancer risk factors. Reducing or eliminating these habits is a powerful step toward long-term health. If you’re over 40, have a family history of cancer, or fall into a higher risk category due to weight or reproductive history, early and regular mammograms are key. As a breast cancer doctor in Hyderabad, I recommend that women schedule screenings tailored to their individual risk. Why Choose Dr. Saadvik Raghuram for Breast Cancer Care in Hyderabad? With years of experience and a patient-first approach, I strive to offer compassionate, evidence-based care at every step of the cancer journey. Whether you are seeking breast cancer treatment, a second opinion, or preventive guidance, I am committed to helping women across Hyderabad live healthier, informed lives. At my clinic, we combine the latest medical advancements with personalized care strategies. I work closely with each patient to understand their lifestyle, risk factors, and concerns, offering not just treatment, but partnership and support. ⸻ Book Your Consultation with Dr. Saadvik Raghuram – Best Breast Cancer Specialist in HyderabadEarly action saves lives. If you’re concerned about your risk or have questions about breast health, schedule a consultation today. About Dr. Saadvik RaghuramDr. Saadvik Raghuram is one of the top-rated oncologists in Hyderabad, specializing in breast cancer treatment and preventive oncology. With a strong academic background and a patient-centered approach, he has helped thousands of patients navigate cancer with clarity, courage, and clinical excellence.
Busting Myths About Ovarian Cancer: What Every Woman Should Know By Dr. Saadvik Raghuram | Medical Oncologist | World Ovarian Cancer Day 2025

Each year, over 300,000 women around the world are diagnosed with ovarian cancer. It’s often called the “silent killer” — not because it strikes without warning, but because its warnings are too often dismissed. This World Ovarian Cancer Day, it’s time we clear the air around ovarian cancer by busting the most common myths — with facts backed by medical research and clinical experience. Myth 1: Ovarian cancer only affects older women. The truth: While the risk increases with age, particularly after menopause, ovarian cancer can occur at any age. According to the American Cancer Society, although the median age of diagnosis is 63, about 15% of cases occur in women under 45. Certain types of ovarian cancer, such as germ cell tumors, are more common in younger women, including teenagers. Takeaway: Age is a risk factor, not a guarantee. Every woman should stay aware of the symptoms. Myth 2: You’ll have clear symptoms if you have it. The truth: Ovarian cancer symptoms are often subtle and nonspecific, which is why nearly 70% of cases are diagnosed at an advanced stage. Common symptoms include: These signs often mimic digestive issues, PMS, or urinary tract infections. Takeaway: If these symptoms persist for more than two weeks, consult a doctor — especially if they are new and unusual for you. Myth 3: PAP smears detect ovarian cancer. The truth: PAP tests screen for cervical cancer, not ovarian. There is no standardized screening test for ovarian cancer yet. While transvaginal ultrasounds and CA-125 blood tests can aid in investigation, they are not recommended for general screening due to false positives and low sensitivity in early stages. Takeaway: A normal PAP smear does not mean you’re clear of ovarian cancer. Myth 4: There’s no hope if you’re diagnosed. The truth: When detected early, ovarian cancer is highly treatable. The 5-year survival rate for Stage I ovarian cancer exceeds 90%. Modern treatments — including targeted therapy, immunotherapy, PARP inhibitors, and refined surgical techniques — have significantly improved outcomes even in later stages. Takeaway: Early detection gives women a fighting chance. New treatment options are more promising than ever. Myth 5: It’s too rare to worry about. The truth: Ovarian cancer is the fifth leading cause of cancer death in women worldwide, making it a major public health concern. According to Globocan (2024), over 313,000 women were diagnosed globally, with ~207,000 deaths. Its lethality is often due to late-stage diagnosis, not rarity. Takeaway: Ovarian cancer is less talked about, not less dangerous. So, what can you do? In Closing: On this World Ovarian Cancer Day, let’s break the silence — and the myths — around this disease. Awareness is the first step toward prevention, early detection, and life-saving care. If you have concerns about ovarian cancer or want to assess your risk, feel free to schedule a consultation with Dr. Saadvik Raghuram. Because every woman deserves to know the truth — and get the care she needs.
How Cancer Treatment Is Evolving in 2025 — And Why That Should Give Us Hope

Cancer care in 2025 is not what it was even five years ago. Today, we are witnessing a powerful shift from broad, aggressive treatments to highly personalized, precision-based therapies that offer better outcomes with fewer side effects. Driven by advancements in immunology, molecular diagnostics, artificial intelligence, and a renewed focus on mental health, cancer treatment is entering a new era—one where survival and quality of life are improving hand-in-hand. Here are five major innovations shaping cancer care in 2025—and why they matter. 1. Immunotherapy Is Getting Smarter Immunotherapy has been one of the most transformative breakthroughs in oncology over the past decade. In 2025, it continues to evolve. Current research focuses on cancer vaccines—not just preventive, but therapeutic vaccines that train the immune system to recognize and remember cancer cells, reducing the chances of recurrence. Innovations like neoantigen vaccines (personalized to a patient’s tumor mutations) and bispecific antibodies are making immune responses more targeted and durable. Research Insight: A study published in Nature (2024) showed that personalized mRNA cancer vaccines, when combined with checkpoint inhibitors, significantly improved progression-free survival in patients with advanced melanoma. 2. Liquid Biopsies Are Revolutionizing Early Detection Liquid biopsies—simple blood tests that detect cancer DNA—are becoming more accurate and accessible in 2025. These tests can now identify early-stage cancers before symptoms appear, enabling interventions when tumors are most treatable. Research Insight: The multi-cancer early detection (MCED) test Galleri has expanded its clinical validation, with new trials showing detection accuracy for over 50 cancer types, often at early stages. This technology has the potential to transform cancer from a late-stage diagnosis into an early intervention—especially for high-risk populations. 3. AI Is Personalizing Treatment Plans Like Never Before Artificial intelligence is now deeply embedded in oncology workflows—from imaging analysis and genomics to predicting treatment responses. AI platforms can rapidly process a patient’s tumor genomics and match them with the most effective treatment protocols, sometimes identifying rare or trial-based therapies not previously considered. Research Insight: A 2024 JAMA Oncology review found that AI-assisted treatment planning improved clinical decision accuracy by 33% and reduced time-to-treatment by 45%, especially in complex cases. 4. Less Chemotherapy, More Precision Medicine While chemotherapy remains vital in many cancer protocols, 2025 is seeing a clear shift toward targeted therapies that spare healthy tissue. Drugs like tyrosine kinase inhibitors, PARP inhibitors, and monoclonal antibodies are designed to target specific mutations or cellular pathways within cancer cells, reducing collateral damage and improving patient quality of life. Research Insight: Clinical trials from ASCO 2024 demonstrated that precision-targeted therapies led to higher response rates and fewer grade 3–4 side effects compared to traditional chemo in certain breast and lung cancers. 5. Mental Health Is Now Part of the Cancer Protocol In 2025, mental health is finally being integrated into oncology care—not as an afterthought, but as a core pillar of treatment. Cancer affects more than just the body, and addressing the psychological and emotional toll is crucial for patient outcomes. Multidisciplinary cancer care teams now include psycho-oncologists, counselors, and social workers as standard practice. Research Insight: A meta-analysis in The Lancet Psychiatry (2023) confirmed that integrating mental health care into oncology reduced treatment non-compliance by 25% and improved survival outcomes in patients with major depressive symptoms. Conclusion: From Hope to Reality These advances aren’t theoretical—they’re happening right now. We are moving from a model of “treating disease” to one of “understanding and managing patients” in the most comprehensive way possible. As a medical oncologist, it’s incredibly promising to see treatments that are not only more effective, but also more compassionate, data-driven, and centered around the individual.Cancer care is changing. And so are the outcomes. If you or a loved one is navigating a cancer diagnosis, know that there is real reason for hope—grounded in science, innovation, and a global commitment to better care. — Dr. Saadvik Raghuram YHOD Medical Oncology | Advocate for Precision Oncology & Holistic Care

